Direct to Consumer Pharma – Growing Importance of Patient-Centric Distribution
Direct to consumer pharma is changing the way patients experience healthcare. For years, people had little knowledge that how medicines reached them. Prices were unclear, the supply chain was long, and patients were left with almost no control. That is beginning to change. By working directly with patients, drug makers can cut through the confusion, offer fairer access, and build stronger trust. The model also gives companies something they never had before: real insight into how patients actually use their medicines. From adherence to outcomes, this feedback helps shape new treatments and better support systems, making the entire process more transparent and patient focused.
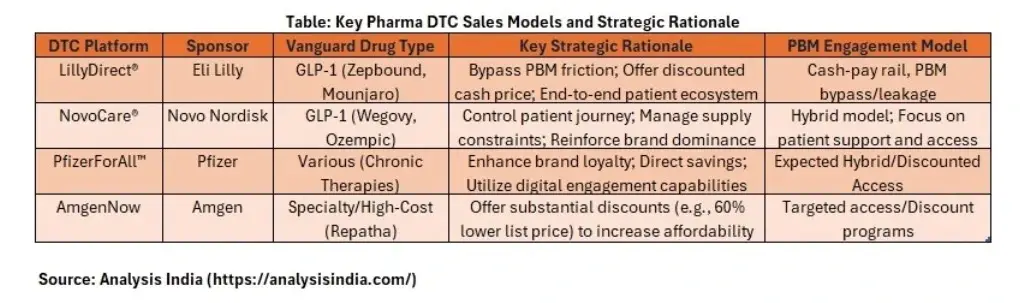
Lessons from Early Direct to Consumer Pharma Leaders
The first wave of direct to consumer initiatives in healthcare shows both the promise and the hurdles of this new model. Pfizer has invested in digital platforms that not only educate patients but also make it easier to access therapies, proving that convenience and knowledge can improve adherence. Eli Lilly has taken a different approach by selling insulin directly at lower prices, showing how cutting out middlemen can make treatment more affordable while also building public trust. At the same time, telehealth companies such as Hims and Hers and Ro are demonstrating the power of combining virtual consultations with direct delivery of medicines, creating a smooth and modern experience that appeals to today’s consumers. Together, these examples make it clear that success in direct to consumer pharma is not just about putting drugs online. It requires a careful balance of innovative pricing, smart use of technology, and a foundation of patient trust.
Policy Reforms as a Catalyst for Direct to Consumer Pharma Growth
Inflation Reduction Act and Drug Pricing Reform
The Inflation Reduction Act has given Medicare the power to negotiate prices for certain high‑cost drugs. This marks a historic shift in United States pharmaceutical policy. For drug makers, it means tighter margins and a strong incentive to explore new revenue models. Direct to consumer strategies are emerging as one way to maintain profitability while it also building patient loyalty.
Most Favored Nation Rule and Global Price Benchmarking
The Most Favored Nation rule, though still debated, reflects a broader push to align U.S. drug prices with those in other developed nations. If implemented, it could significantly reduce profit margins in the American market. To adapt, companies may cut distribution costs and move closer to patients by bypassing traditional intermediaries.
The 340B Program and Market Distortions
The 340B program requires manufacturers to provide discounted drugs to eligible healthcare providers. While designed to support underserved communities, it has also created pricing distortions and tensions between manufacturers and providers. Direct to consumer models offer a way for companies to regain control over pricing and distribution while reducing reliance on complex compliance structures.
A Catalyst for Innovation
Taken together, these reforms are not just constraints. They are catalysts that are reshaping incentives across the industry. By pushing companies toward more transparent, efficient, and patient‑focused models, policy changes are accelerating the shift to direct-to-consumer healthcare.
How Patient Expectations Are Driving the Direct to Consumer Pharma Revolution
Patient expectations are reshaping the direct to consumer shift in healthcare. The pandemic pushed digital health into daily life, with telemedicine, online pharmacies, and app-based tools becoming routine. People now expect healthcare to match the convenience and personalization they get from e commerce. They want clear prices, quick access to consultations, and support that fits their routines. This cultural change is a powerful force behind the rise of direct to consumer models. Patients are asking for care that is accessible, transparent, and built around their needs, and the industry is starting to respond.
Risks and Challenges of Direct to Consumer Pharma Models
Direct to consumer pharma brings real possibilities, but it also comes with risks that cannot be ignored. Regulators continue to scrutinize how prescription drugs are marketed directly to patients, and equity is a concern when digital first models leave out people without stable internet access or the skills to navigate online tools. Protecting patient data is a major responsibility, since companies must use sensitive information to personalize care while keeping it secure. Tensions can also arise with traditional players such as pharmacies and benefit managers who may resist being bypassed. And while easier access can be a benefit, it can also fuel overuse or unnecessary consumption. To earn trust and deliver value, companies need to pair innovation with strong safeguards, responsible practices, and clear guardrails.
Direct to Consumer Pharma – Understanding Patient Behavior and Cost Sensitivity
Patient behavior sits at the core of direct to consumer healthcare. Studies show that patients are highly sensitive to out of pocket costs, and even small reductions can improve adherence. Trust matters just as much. People are more likely to stay engaged with brands that are transparent, empathetic, and reliable. Convenience alone does not sustain adherence over time. Continuous engagement through education, timely reminders, and accessible support is essential for long term treatment success. Preferences also differ by age and context, with younger patients tending to favor app-based interactions and older patients often choosing hybrid models that blend digital tools with familiar, face to face support.
The Future of Direct to Consumer Pharma Models
The future of direct to consumer pharma will be defined by deeper ties to digital health. Wearables, remote monitoring, and artificial intelligence will help build a complete patient journey that goes beyond a single prescription and supports care over time. The United States leads today, but fast growing markets such as India and Southeast Asia are set to adopt these models quickly as their digital health infrastructure expands. In practice, the next phase is likely to be a hybrid approach that blends traditional distribution with direct engagement, giving patients the benefits of both systems. Policy will evolve alongside these changes. Regulators are expected to introduce new frameworks that encourage innovation while protecting patients and their data. At its core, the rise of direct to consumer models reflects a wider shift toward patient empowerment. People want more control over their health decisions, and companies are responding with care that is more accessible, more affordable, and more personalized.